You finish lunch, ready to tackle the day—but instead, your energy plummets. That heavy-lidded sensation many experience after meals often sparks quiet worry. Could this common slump signal something more serious? While occasional drowsiness is normal, recurring fatigue paired with other symptoms might warrant deeper exploration.
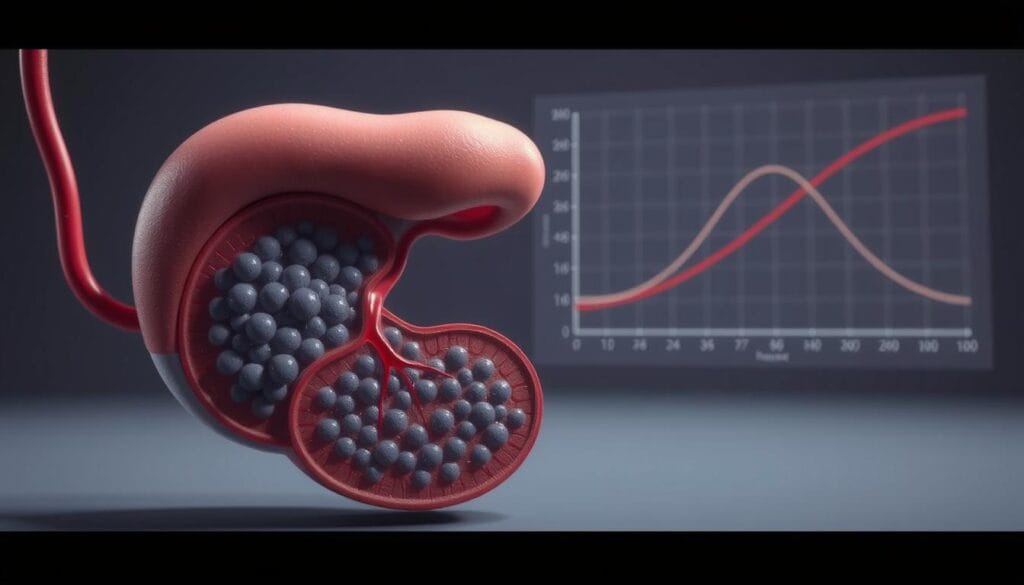
Carbohydrate-rich meals trigger a natural chain reaction. The body breaks down sugars, releasing glucose into the bloodstream. Insulin then helps cells absorb this energy source. However, sharp spikes followed by rapid drops can leave individuals drained. Research shows one in ten Americans manages diabetes, a condition disrupting this delicate balance.
Multiple factors contribute to post-meal tiredness. Overeating strains digestion, while dehydration reduces metabolic efficiency. Even food choices matter: processed snacks cause quicker crashes than fiber-rich alternatives. Vegetables and whole grains promote steadier glucose levels, supporting sustained vitality.
Though fatigue alone rarely confirms diabetes, understanding patterns matters. Persistent thirst, unexplained weight changes, or blurred vision alongside exhaustion could indicate blood sugar irregularities. Consulting healthcare professionals ensures accurate assessment—early intervention prevents complications.
Key Takeaways
- Post-meal fatigue is common but rarely alarming when occasional
- Blood sugar fluctuations influence energy levels after eating
- Diet composition affects how the body processes carbohydrates
- Diabetes impacts 10% of Americans, making awareness crucial
- Multiple symptoms combined warrant medical consultation
Understanding Post-Meal Sleepiness and Its Causes
Imagine savoring a hearty meal, only to battle heavy eyelids moments later. This phenomenon stems from two interconnected systems: blood sugar regulation and digestive energy demands. While temporary drowsiness is normal, recurring patterns may reveal how the body manages fuel distribution.
Role of Blood Sugar Changes
Carb-heavy meals trigger a glucose surge, prompting the pancreas to release insulin. This hormone escorts sugar into cells for energy production. However, overshooting insulin levels can create a subsequent crash, leaving individuals drained. A 2021 Nutrition Journal study found participants consuming high-glycemic meals experienced 23% greater fatigue than those eating balanced options.
The speed of carbohydrate breakdown matters. Simple sugars flood the bloodstream rapidly, while whole grains release glucose gradually. This difference explains why a candy bar provides fleeting energy compared to oatmeal’s sustained vitality.
Impact of Digestive Processes on Energy Levels
Digestion consumes roughly 10% of daily energy expenditure. After large meals, blood flow prioritizes the gut over other organs. This shift can temporarily reduce cerebral oxygen supply, amplifying tiredness. Spicy or fatty foods intensify this effect by prolonging digestion time.
Individual biology plays a key role. People with efficient metabolisms often rebound quicker from energy dips. Conversely, those with insulin resistance may experience prolonged sluggishness. Tracking food choices alongside energy levels helps identify personal triggers.
Examining the Link: is feeling sleepy after eating a sign of diabetes
While occasional tiredness post-meal raises questions, diabetes reveals itself through multiple concurrent signals. Sleepiness alone rarely confirms the condition, but paired with other patterns, it may indicate metabolic irregularities needing professional evaluation.
Identifying Diabetic Symptoms Beyond Sleepiness
Diabetes often announces itself through distinct physical changes. Unexplained weight loss occurs when cells can’t access glucose, forcing the body to burn fat and muscle. Excessive thirst and frequent urination develop as kidneys work overtime to filter excess blood sugar. Blurred vision and persistent dry skin further signal prolonged glucose imbalances.
Key markers like tingling hands or feet suggest nerve damage from chronic high glucose levels. These symptoms typically appear together, creating a clearer diagnostic picture than isolated fatigue.
How Insulin Response Affects Post-Meal Energy
In non-diabetic individuals, insulin efficiently transports glucose into cells. Those with type 1 diabetes produce little to no insulin, while type 2 diabetes involves insulin resistance. Both scenarios leave glucose stranded in the bloodstream instead of fueling cells.
Post-meal energy crashes intensify when insulin can’t stabilize blood sugar levels. A 2023 Clinical Diabetes study noted that individuals with uncontrolled diabetes experienced glucose spikes 58% higher than healthy counterparts after identical meals. This imbalance explains why exhaustion often follows eating in undiagnosed cases.
Accurate diagnosis requires testing fasting glucose levels and HbA1c averages. Early intervention helps prevent complications, making symptom awareness vital for long-term health management.
Exploring Other Factors Affecting Energy Levels After Meals
Meal choices and daily routines play pivotal roles in determining how energized one feels after eating. While blood sugar management remains crucial, multiple overlapping elements influence post-meal vitality.

Influence of Meal Composition and Portion Size
Foods rich in simple carbohydrates—like white bread or sugary snacks—trigger rapid glucose spikes followed by crashes. A balanced diet incorporating proteins, healthy fats, and fiber slows digestion, promoting steadier energy release. For example:
| Meal Component | Energy Impact | Examples |
|---|---|---|
| Simple Sugars | Quick spike, rapid crash | Candy, soda |
| Complex Carbs | Sustained release | Quinoa, lentils |
| Proteins/Fats | Slow absorption | Almonds, grilled chicken |
Larger portions demand more digestive effort. “Overeating activates the parasympathetic nervous system, redirecting blood flow to the stomach,” explains a 2022 Gastroenterology Report. This shift can temporarily reduce alertness.
Lifestyle Contributors: Sleep, Exercise, and Hydration
Sleep quality directly affects daytime energy reserves. Adults averaging under seven hours nightly experience 34% higher fatigue rates post-meal, per Sleep Health Journal data. Regular exercise enhances metabolic efficiency—even light activity like walking improves glucose uptake by muscles.
Hydration also matters. Water aids nutrient transport and waste removal, while dehydration slows cellular energy production. Pairing these habits with mindful eating creates a foundation for sustained vitality throughout the day.
The Science Behind Blood Sugar, Insulin, and Sleep
From plate to cell, meals orchestrate intricate energy pathways. Three key players—glucose, insulin, and circadian rhythms—determine how food converts to vitality or fatigue. This biological interplay explains why some meals fuel productivity while others invite drowsiness.
Understanding Glucose Fluctuations After Eating
Carbohydrates break down into glucose during digestion, entering the bloodstream within minutes. Simple sugars cause rapid spikes, while complex carbs release energy gradually. This difference creates distinct patterns:
| Food Type | Glucose Rise | Energy Duration |
|---|---|---|
| White Bread | Sharp peak (30 mins) | 1-2 hours |
| Sweet Potato | Gradual incline | 3-4 hours |
A 2023 Metabolism Journal study found participants with stable sugar levels reported 42% less daytime fatigue. Dramatic drops after spikes—often called “sugar crashes”—occur when excess insulin overcorrects high glucose levels.
The Role of Insulin in Energy Regulation
Insulin acts as a cellular gatekeeper, allowing glucose to enter muscles and organs. Efficient absorption maintains energy balance. However, repeated sugar surges can dull insulin sensitivity over time.
Research links consistent blood sugar management to deeper sleep cycles. “Cells function optimally when fuel arrives steadily, not in bursts,” notes endocrinologist Dr. Lisa Yang. Nighttime glucose stability reduces sleep disruptions, creating a virtuous cycle for metabolic health.
Understanding these mechanisms empowers better meal timing and composition choices. Pairing proteins with carbs slows digestion, while regular activity enhances insulin efficiency—simple strategies for sustained vitality.
Nutritional Strategies to Prevent Post-Meal Fatigue
Smart food choices transform meals from energy drains to vitality boosters. Research reveals that carbohydrate quality significantly impacts blood sugar management. A 2023 Journal of Nutritional Science study found participants prioritizing complex carbs reported 37% less afternoon fatigue than those consuming refined sugars.
Carbohydrate Quality Matters
Complex carbohydrates break down slowly due to their fiber content and molecular structure. This gradual digestion prevents sudden glucose surges, supporting stable energy levels for hours. Whole grains, legumes, and non-starchy vegetables rank among the most effective options.
Compare these common foods:
| High-GI Choices | Low-GI Alternatives | Glycemic Index |
|---|---|---|
| White rice | Quinoa | 53 vs 35 |
| Instant oatmeal | Steel-cut oats | 79 vs 55 |
| Russet potato | Sweet potato | 111 vs 70 |
Pairing carbs with proteins or healthy fats enhances stability. Nutritionist Dr. Elena Martinez notes: “Adding avocado to whole-grain toast slows glucose absorption by 40%, extending energy release.”
Practical dietary shifts yield lasting benefits. Swapping sugary snacks for roasted chickpeas or choosing brown rice over white creates sustained fuel. Tracking energy patterns after meals helps identify optimal food combinations for individual needs.
These strategies form part of a proactive approach to metabolic health. Consistent choices support blood sugar balance while reducing reliance on stimulants like caffeine. Over time, this dietary framework promotes both immediate vitality and long-term wellness.
Lifestyle Changes for Better Energy and Overall Health
Sustainable energy management extends beyond meal choices into daily habits. Combining nutritional strategies with intentional routines creates a synergistic effect, enhancing both immediate vitality and long-term well-being.
Enhancing Sleep Quality and Incorporating Physical Activity
Adults prioritizing 7-8 hours of nightly sleep show 40% fewer midday energy crashes, per Sleep Research Society data. Consistent bedtimes and dark, cool environments improve sleep architecture. “Quality rest optimizes cellular repair and glucose metabolism,” notes neurologist Dr. Rachel Torres.
Regular movement proves equally vital. The CDC recommends 150 weekly minutes of moderate exercise—a target achievable through brisk walking or cycling. Strength training twice weekly further enhances insulin sensitivity, helping muscles utilize glucose efficiently.
Diet Adjustments and Reducing Alcohol Consumption
Gradual dietary changes yield lasting results. Swapping sugary drinks for herbal tea or reducing processed snacks by 20% weekly can stabilize blood sugar. Alcohol moderation remains critical—research links two daily drinks to 27% higher glucose variability.
Practical strategies for different needs:
- Non-diabetic individuals: Start with 1 alcohol-free day weekly
- Those managing health conditions: Explore mocktails using sparkling water and citrus
These lifestyle adjustments benefit all people, particularly people diabetes seeking improved glycemic control. Small, consistent modifications create compounding energy benefits while supporting metabolic health.
Conclusion
Post-meal fatigue often sparks concern but rarely stands alone as a health indicator. Multiple factors—from meal size to hydration—influence energy crashes. Blood sugar fluctuations remain central, with sharp spikes triggering insulin surges that may drain vitality.
While diabetes can amplify these patterns, diagnosis requires multiple symptoms like frequent urination or unexplained weight shifts. The CDC reports 9.4% of U.S. adults manage this medical condition, highlighting the need for professional evaluation when patterns persist.
Nutritional adjustments and activity timing offer practical solutions. Choosing complex carbs over sugary snacks stabilizes glucose levels, while hydration supports metabolic efficiency. Even minor lifestyle shifts—like post-meal walks—enhance insulin sensitivity.
Ultimately, understanding the body’s signals proves vital. Those experiencing recurring tiredness alongside other changes should prioritize clinical consultation. Proactive management combines informed choices with medical guidance—a balanced approach to sustaining energy and overall health.
FAQ
Can post-meal sleepiness indicate diabetes?
Persistent fatigue after eating may signal blood sugar dysregulation, a hallmark of type 2 diabetes. When insulin resistance prevents glucose from entering cells effectively, energy crashes often follow meals. However, this symptom alone doesn’t confirm diabetes—medical testing is required for diagnosis.
What other diabetes symptoms accompany post-meal fatigue?
Beyond tiredness after eating, common signs include excessive thirst, frequent urination, blurred vision, and unexplained weight changes. The American Diabetes Association emphasizes that consistently high blood glucose levels (above 126 mg/dL fasting) are key diagnostic markers.
How do carbohydrate-rich meals affect energy levels?
Meals high in simple carbohydrates like white bread or sugary snacks cause rapid glucose spikes, followed by insulin surges that can lead to reactive hypoglycemia. This rollercoaster effect often results in pronounced fatigue 1-3 hours after eating.
Can lifestyle changes reduce post-meal sleepiness?
Yes. Prioritizing 7-9 hours of quality sleep nightly, engaging in 150 minutes of weekly aerobic exercise (per CDC guidelines), and staying hydrated help stabilize blood sugar levels. Pairing carbs with protein or healthy fats also slows glucose absorption.
How does insulin resistance contribute to fatigue?
In insulin-resistant individuals, cells struggle to utilize glucose efficiently despite adequate insulin production. This mismatch leaves cells energy-starved while excess glucose circulates in the bloodstream—a dual mechanism that exacerbates post-meal tiredness.
Are certain foods better for preventing energy crashes?
Fiber-rich complex carbohydrates like quinoa, legumes, and whole grains cause slower glucose release compared to refined carbs. Adding lean proteins (chicken, tofu) and monounsaturated fats (avocados, nuts) further stabilizes energy levels after meals.
When should someone consult a doctor about post-meal fatigue?
Medical evaluation is recommended if fatigue persists despite dietary adjustments, or if accompanied by classic diabetes symptoms. An A1C test measuring average blood sugar levels over 3 months provides clearer diagnostic insights than single glucose readings.
Source Links
- Is Feeling Sleepy After Eating a Sign of Diabetes?
- Feeling Sleepy After Eating Could Be Diet, Not Diabetes
- Is Falling Asleep After Eating a Sign of Diabetes?
- Is Feeling Sleepy After Eating a Sign of Diabetes?
- Is Falling Asleep After Eating a Sign of Diabetes?
- Why Do I Get Tired After Eating? Symptoms of Fatigue
- Is Falling Asleep After Eating a Sign of Diabetes? – Healthcare Associates of Texas
- Is Falling Asleep After Eating a Sign of Diabetes? – Circufiber
- Is Falling Asleep after Eating a Sign of Diabetes? – Lorena Drago, MS, RDN, CDN, CDE
- Here’s Why You Get Sleepy After Eating
- Is Falling Asleep After Eating a Sign of Diabetes?
- Is Falling Asleep After Eating a Sign of Diabetes? | Nourish
- Is Feeling Sleepy After Eating a Sign of Diabetes? 6 Facts to Know
- The Link Between Sleeping and Type 2 Diabetes: A Systematic Review
- Does High Blood Sugar Make You Sleepy? What You Must Know | Signos
- 6 simple ways to prevent blood sugar spikes after meals
- What are the Best and Worst Foods to Balance Blood Sugar?
- Diabetes management: How lifestyle, daily routine affect blood sugar
- Healthy Living with Diabetes – NIDDK
- Is Falling Asleep After Eating a Sign of Diabetes? – Circufiber
- Is Falling Asleep After Eating a Sign of Diabetes? Causes and Solutions


























